By Haroon Rashid
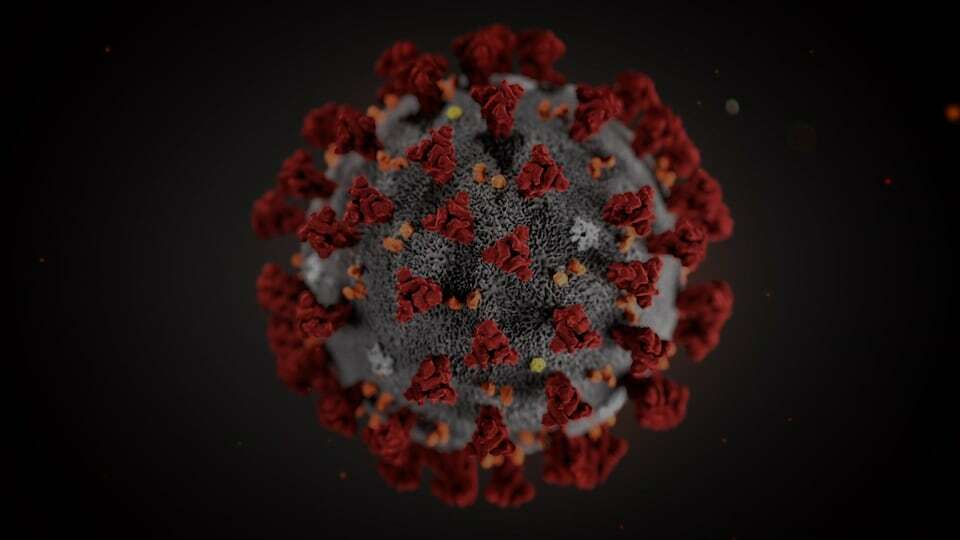
The global pandemic of novel coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and was first detected in early December 2019 in Wuhan, China, spreading worldwide thereafter. Till date, more than 2.7 million individuals have been affected worldwide and causing nearly 1.9 lakh deaths.
The novel coronavirus has taken just a few months to sweep the globe. It is kind of a perfect storm, difficult to track and control and is severe enough to kill a significant fraction of those who have it.
Covid-19 is spreading rapidly, and at the moment, we are relying on quarantine, isolation, and infection-control measures to prevent disease spread, and providing supportive care for those who are infected. We lack a specific anti-viral agent to treat the infected and, optimally, decrease viral shedding and subsequent transmission. Modern medicine has so much, yet so little, to offer, when it comes to this pesky little virus. A number of drugs in the pipeline are undergoing evaluation in clinical trials, although their clinical effectiveness has not been fully evaluated yet. As of now, there is no evidence from randomized clinical trials (RCTs) that any potential therapy improves outcome in patients with either suspected or confirmed COVID-19.
Any intervention that lacks data supporting clinical use should not hastily be assumed to be efficacious. Administration of any unproven drug as a “last resort” wrongly assumes that the benefits will overshadow the harm, and physicians must exercise caution in this context. When a drug with unknown clinical effects is prescribed to patients suffering from a novel disease such as COVID-19, there is no way to know whether the patients shall be benefited or harmed in the absence of a concurrent control group, not to mention the unintended consequences, including a rise in resistance to these compounds by parasites and bacteria, their original intended targets.
The dangers posed by hasty use of repurposed drug Hydroxychloroquine (HCQ) for COVID-19 is a case in point. Chloroquine and hydroxychloroquine are widely used as anti-malarial drugs, and for treatment of autoimmune disorders. HCQ is a more soluble, and less toxic, metabolite of chloroquine, causing fewer side effects and is, therefore, considered safer. It has been reported that HCQ inhibits ACE2 receptor-mediated entry of the SARS-CoV-2 virus through various actions such as increasing endosomal pH, inhibiting lysosomal activity, affecting antigen processing, etc. In addition, it has anti-inflammatory and immunomodulatory effects, which could be relevant in the crisis generated by cytokines storm during COVID-19 infection.
HCQ is currently being used globally for treatment and prophylaxis of COVID-19, despite weak evidence of its effectiveness, and despite causing, apparently, serious adverse events, including -QT interval prolongation and Torsade de pointe, hypoglycaemia, mental status changes and psychosis, drug-drug interaction, haemolysis (rare), and retinopathy. HCQ turned into a COVID-19 ‘wonder drug’ after it was demonstrated to have anti-SARS-CoV activity in vitro, regardless of the fact that the available in vivo data was limited to few studies, with very small sample sizes, a number of methodological flaws, and conflicting results. Report of their benefits in patients comes from 1 press release for a trial in China and 1 preprint case series.
A French non-randomized open-label trial, published in preprint, reported a significant decrease in viral load and carriage duration in COVID-19 patients receiving HCQ, with enhanced effects in combination with azithromycin. Although the results of these clinical trials sound promising, this study also has major limitations including small sample size, no intention-to-treat analysis, no analysis of clinical benefits, and only short-term follow-up. In short, the evidence provided by this study supporting use of HCQ to treat COVID-19 is, at best, flimsy.
Despite these substantial limitations, misinterpretations of the results claiming effectiveness of HCQ in treatment of COVID-19 patients spread spectacularly quickly through internet, social media, television news, and the press, and were endorsed by many government and institutional leaders including President Trump who referred to this as a “game changer”. Consequently, public interest in HCQ rapidly grew, and people, frightened by COVID-19, began hoarding these drugs, at the risk of misuse and overdose.
The US Food and Drug Administration (USFDA), on March 28th this year, granted emergency authorization to clinicians to prescribe HCQ for treatment of COVID-19. The agency acknowledged that the approval was based on “limited in-vitro and anecdotal clinical data”. On the basis of preliminary results from ongoing clinical trials, some countries have incorporated HCQ into their treatment protocols for certain patients with COVID-19 or as prophylaxis for health care workers at risk. Subsequently, Indian Council of Medical Research (ICMR) also recommended the use of HCQ for prophylaxis of SARS-CoV-2 for high risk population, but not for general public.
As more studies roll in, little evidence is in favour of hydroxychloroquine.According to a recent retrospective study of 368 Veterans Affairs (VA) patients hospitalized with COVID-19, the researchers found “no evidence that use of hydroxychloroquine, either with or without azithromycin, reduced the risk of mechanical ventilation” in the COVID-19 patients. Nearly 28 percent of those who got the hydroxychloroquine died, and 22.1 percent of those with the combination died, while only 11.4 percent died among those who got neither.This study too had limitations. It was retrospective, non-randomised study; the patients who received HCQ were more severely ill and only male veterans were included. The study has not yet been peer-reviewed.
We must remember that the use of repurposed medication relies on the assumption that the benefits (in vitro/clinical evidence) outweigh associated risks (adverse drug reactions). In using repurposed drugs, caution must be exercised, because several treatments that initially seem “promising” later prove to be harmful, as evident by the withdrawal of a number of medicines due to adverse reactions despite showing promising clinical outcomes. No drug is guaranteed to be 100% safe, and indiscriminate usage of HCQ will expose some patients to potentially fatal adverse events. To make matters worse, some people are already attempting to self-medicate with the drug, with disastrous consequences. Thus, off-label use of HCQ must be discouraged until justified with adequate evidence, and production levels boosted. If the current trend continues, HCQ shortage not only will limit availability to patients with COVID-19 if efficacy is truly established but also patients with rheumatic diseases who depend on HCQ for their survival.
Public figures should refrain from promoting unproven therapies to the public and, instead, provide clear messages about the uncertainties around testing and use of experimental treatments during the current pandemic, including the risk of serious adverse events. In a recent White House press briefing President Donald Trump suggested injecting people with ‘DISINFECTANT’ and hitting ‘the body with a very powerful light’ can cure people with COVID-19. Such hasty and inappropriate interpretation of scientific literature by public leaders has the potential to do serious harm. Clinicians also need not to prescribe HCQ indiscriminately in a desperate attempt to fight COVID-19, despite the absence of robust evidence to support their clinical benefits.
In conclusion, at present, except for supportive measures, infection with SARS-CoV-2 is “essentially untreatable.” Since there is insufficient data to “recommend either for or against” hydroxychloroquine, we urgently need well designed, properly powered, randomised controlled trials of HCQ and till then these drugs should be prescribed cautiously, with initial cardiac evaluation in outpatients, daily ECG, and twice-weekly residual blood concentration monitoring of hospitalized patients. Even though FDA granted authorization for emergency use, and ICMR also recommended it for prophylaxis of COVID-19 in high risk groups, clinicians must conduct rigorous benefit-risk assessment of each individual case, and seek better evidence before routinely using these drugs to treat patients with COVID-19.
(The author is pursuing PhD in the Department of Pharmacology, All India Institute of Medical Sciences New Delhi)