By Mahpara Mushtaq
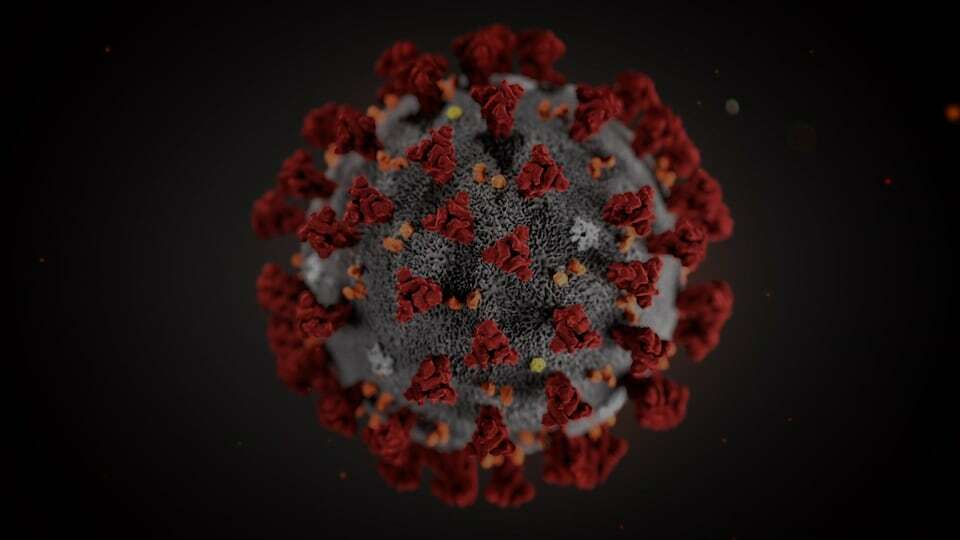
Coronavirus also known as COVID-19 is a pandemic disease that needs no introduction. The disease has globally affected more than 700,000 people and among these 31,737 died due to it.
In India alone, cases have surged past 1000 with at least 25 people losing their lives. These numbers change rapidly and must have changed while these lines were being written.
Although a novel or new disease it is, it has made the people in our part of the world familiar to the ideas of isolation and quarantine. To begin with, let’s try to understand what these terms mean.
While the individuals are obliged to protect others by adhering to isolation guidelines and at the same time the state is also obliged to provide better facilities to the individuals. In order to contain the progression of COVID-19 pandemic, the role of both the players is a must at this stage.
Isolation is most commonly used when a patient is known to have a contagious (transmissible from person-to-person) viral or bacterial illness. Special equipment is used in the management of patients in the various forms of isolation.
These most commonly include items of personal protective equipment (gowns, masks, and gloves) and engineering controls (positive pressure rooms, negative pressure rooms, laminar airflow equipment, and various mechanical and structural barriers). Isolation should not be mistaken as the same as quarantine.
Quarantine is the compulsory separation and confinement, with restriction of movement, of healthy individuals or groups who have potentially been exposed to an agent to prevent further infections should infection occur.
Contagious diseases can spread to others through various forms. Four types of infectious disease transmission can occur:
(1) Contact transmission, which can be through direct physical contact, indirect contact through fomites (mobile phones, handkerchiefs, pens and other potent surfaces) or droplet contact in which airborne infections spread short distances.
(2) Vehicular transmission, which involves contaminated objects.
(3) Airborne transmission, which involves spread of infectious particles through air.
(4) Vector transmission, which is spread through insects or animals.
Depending on the contagious disease, transmission can occur within a person’s home, school, worksite, health care facility, and other shared spaces within the community. Therefore, isolation is an important infection prevention and control practice used to protect others from disease. Isolation can prevent healthcare-acquired infections or hospital-acquired infections (HCAIs), reduce threats of antibiotic resistance infections, and respond to new and emerging infectious disease threats globally.
The U.S. Center for Disease Control and Prevention (CDC) created various levels of disease isolation (also described “precaution”). These precautions are also reviewed and revised by the CDC. Various forms of precaution are as:
Universal/standard precautions:
Universal precautions refer to the practice, in medicine, of avoiding contact with patients’ bodily fluids, by means of the wearing of nonporous articles such as medical gloves, goggles, and face shields. The practice was widely introduced in 1985-88. In 1987, the practice of universal precautions was adjusted by a set of rules known as body substance isolation. In 1996, both practices were replaced by the latest approach known as standard precautions. Use of personal protective equipment is now recommended in all health settings.
Transmission-based precautions
Transmission-based precautions are additional infection control precautions – over and above universal/standard precautions – and the latest routine infection prevention and control practices applied for patients who are known or suspected to be infected or colonized with infectious agents, including certain epidemiologically important pathogens. The latter require additional control measures to effectively prevent transmission. There are three types of transmission-based precaution:
i. Contact precautions are intended to prevent transmission of infectious agents, including epidemiologically important microorganisms, which are spread by direct or indirect contact with the patient or the patient’s environment.
ii. Droplet precautions are intended to prevent transmission of pathogens spread through close respiratory or mucous membrane contact with respiratory secretions.
iii. Airborne precautions prevent transmission of infectious agents that remain infectious over long distances when suspended in the air (e.g., rubeola virus [measles], varicella virus, M. tuberculosis, and possibly SARS-CoV).
Ethics of it
Now coming to the ethical part of it, isolation serves as an important method to protect the general community from the disease, especially in a hospital or community-wide outbreak.
Isolation can be justified as a morally legitimate ethical practice in public health based on the reciprocal relationship between the individual and the state.
The individual is obligated to protect others by preventing further spread of disease, respect the instructions from public health authorities and sequester themselves in their homes and not attend public gatherings, and act as a first responder (if a healthcare professional) by providing services to protect and restore public health.
The state, on the other hand, is obligated to provide support to individuals burdened as a result of restrictive measures (e.g. compensation for missed work, providing access to food and other necessities for those quarantined and isolated, assistance for first responders to balance personal/professional obligations), ensure several legal protections are in place for those subjected to restrictive measures and communicate all relevant information regarding the necessity of restriction.
Contextualizing it with regard to Kashmir, while the individuals are obliged to protect others by adhering to isolation guidelines and at the same time the state is also obliged to provide better facilities to the individuals. In order to contain the progression of COVID-19 pandemic, the role of both the players is a must at this stage.
Author is a registered Nurse in the Department of Social and Preventive Medicine (SPM), GMC Srinagar